Neuroinflammation: How It Shapes Your Brain and Mental Health
Inflammation is a buzzword you might hear often these days, but what does it really mean? Let’s start with the origin of the word: Derived from the Latin word "inflammatio," meaning "to set on fire" or "to ignite," inflammation is associated with redness and warmth that resemble a fire.
While inflammation is typically associated with physical symptoms like swelling and redness, it’s important to understand that inflammation can also be more subtle and occur within the brain. This "invisible fire," known as neuroinflammation, plays a huge role in how we think, feel, and function. From cognitive impairment to mood disorders like anxiety and depression, brain inflammation can have a tremendous impact.
In this article, we’ll explore what inflammation is, how it affects the brain, and—most importantly—the steps you can take to protect and improve your mental health.
What is Inflammation?
Inflammation is a natural response by the immune system when the body detects injury, infection, or other threats. It’s a protective mechanism designed to fight off infections and repair damage. When inflammation occurs, immune cells rush to the affected area, releasing chemicals to neutralize the threat and begin the healing process.
Typical Inflammation
In general, inflammation in the body is characterized by:
Swelling: A visible sign of immune activity.
Sensitivity: The area may feel tender or painful to touch.
Reduced Function: Inflammation can interfere with normal function, like making it harder to move a swollen joint.
This type of inflammation is beneficial for short periods, as it’s part of the healing process. However, when inflammation becomes chronic or unresolved, it can lead to damage.
What is Neuroinflammation?
Neuroinflammation refers to inflammation in the brain or spinal cord. Unlike visible inflammation, neuroinflammation is invisible and causes no direct pain. Instead, it affects the brain's functioning in ways that can significantly alter mood, cognition, and overall mental health.
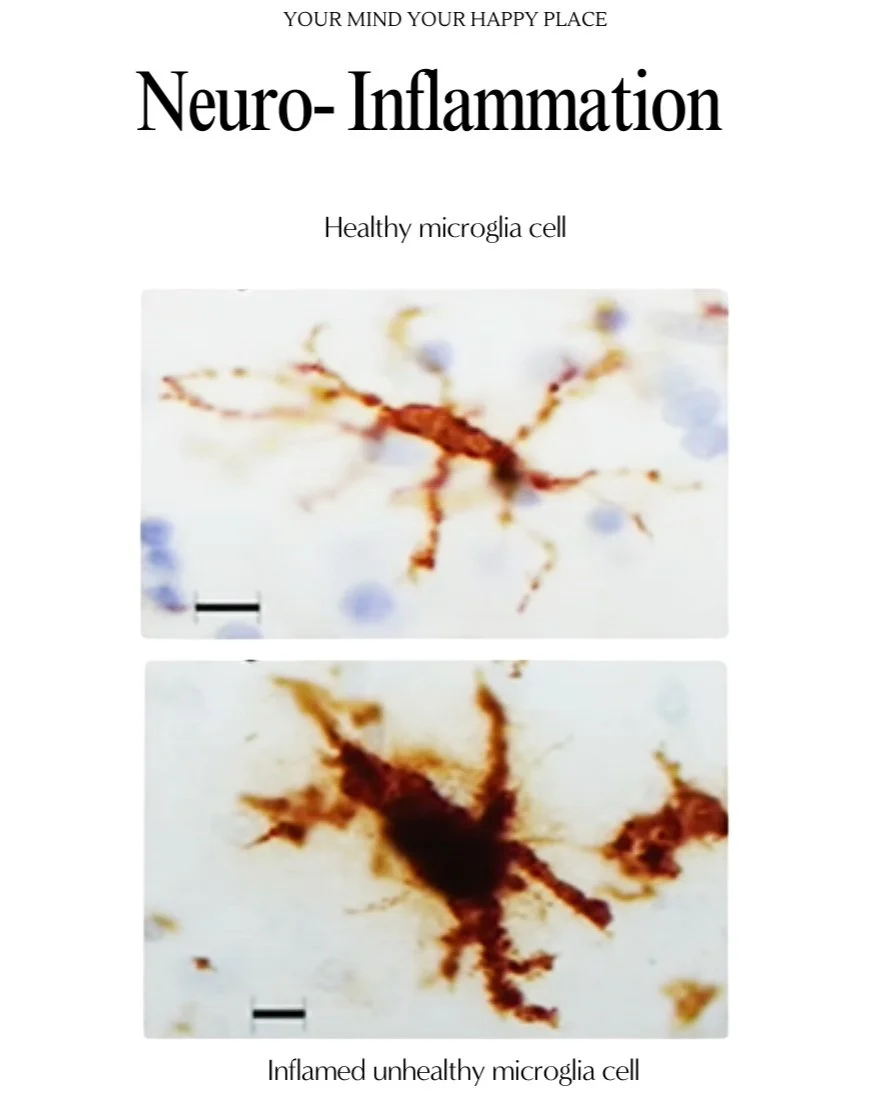
The Brain’s Immune System: Microglia
The brain has its own specialized immune cells, called microglia, which act as its first line of defense. When these cells detect a threat—such as an infection, injury, or chronic stress—they release inflammatory chemicals called cytokines.
While this response is initially protective, excessive or prolonged activation of microglia can lead to chronic neuroinflammation, causing:
Neurodegeneration: Damage to neurons and loss of brain tissue, impairing memory, personality, and decision-making.
Cognitive Impairment: Difficulties with attention, learning, and memory.
Mood Disorders: Increased risk of depression and anxiety due to cytokine dysregulation.
An inflamed microglia cell versus a healthy microglia cell
Causes of Neuroinflammation
1. Infection
Certain infections can invade the central nervous system, triggering a significant inflammatory response.
Examples: Zika virus, fungal toxins (mycotoxins), and parasites like Toxoplasma gondii have all been linked to neuroinflammation and long-term neurological damage.
2. Physical and Emotional Trauma
Physical Trauma: Head injuries or spinal cord injuries can damage brain tissue and activate microglia, leading to inflammation.
Emotional Trauma: Chronic stress or PTSD can disrupt the brain's immune system. Stress hormones trigger an overproduction of pro-inflammatory cytokines, impacting areas of the brain that regulate mood and memory.
3. Lifestyle Factors
Certain habits can increase the risk of neuroinflammation:
Poor Diet: Diets high in processed foods, sugar, and unhealthy fats can lead to systemic inflammation, which often affects the brain.
Lack of Exercise: Regular movement reduces inflammation by improving circulation and enhancing the lymphatic system.
Sleep Deprivation: Poor sleep disrupts the body’s natural inflammatory responses.
Chronic Stress: Long-term stress elevates cortisol levels, which can trigger systemic and neuroinflammation.
Invisible but Impactful: How Neuroinflammation Affects You
Neuroinflammation may not be visible, but its effects on the brain are profound:
Synaptic Disruption: It damages the connections between neurons, affecting how your brain processes information.
Personality and Mood Changes: Chronic inflammation can lead to depression, anxiety, and mood swings.
Progressive Neurological Disorders: It is linked to diseases like Alzheimer’s, Parkinson’s, and Multiple Sclerosis.
“Unlike any other part of the body, if you damage a small piece of the brain, who you are is going to change radically.”
– David Eagleman
How to Protect Your Brain
Taking care of your brain doesn’t require drastic changes. Small, consistent habits can significantly reduce inflammation and improve mental health.
Diet
Eat anti-inflammatory foods like leafy greens, fatty fish rich in omega-3s, nuts, and berries.
Limit or avoid processed foods, sugar, and trans fats, which fuel systemic inflammation.
Movement
Incorporate regular exercise, such as a 30-minute walk or yoga session, to reduce inflammation and improve brain health.
Stress Management
Build resilience to stress by practicing mindfulness, meditation, or engaging in hobbies that relax you.
Sleep Hygiene
Prioritize 7–9 hours of quality sleep each night. Sleep allows the brain to detoxify and repair itself, reducing inflammation.
The Power of Basics in Brain Health
Focusing on simple, everyday habits—like eating well, staying active, managing stress, and getting enough sleep—you can reduce your risk of neuroinflammation. These habits act as medicine, protecting your brain and supporting mental health.
Want to learn more about how brain health connects to your lifestyle? Share your thoughts or questions in the comments below, and let’s start a conversation!
Some sources:
Microglia and Inflammation: Longo, F. M., & Massa, S. M. (2013). Neuroprotective Strategies in Alzheimer's Disease: Role of Microglia and Neuroinflammation.
Link: PubMedNeuroinflammation in Depression and Anxiety
Miller, A. H., & Raison, C. L. (2016). The Role of Inflammation in Depression: From Evolutionary Imperative to Modern Treatment Target.
Link: Nature Reviews Immunology
Connection Between Lifestyle and Inflammation
Calder, P. C., et al. (2017). The Role of Diet in Inflammation: Key Factors Impacting Health and Chronic Diseases.
Link: ScienceDirect
Emotional Stress and Inflammation
Pace, T. W. W., & Miller, A. H. (2009). Cytokines and Glucocorticoid Receptor Signaling: Relevance to Major Depression.
Link: PubMed
Lifestyle and Chronic Inflammation
Medzhitov, R. (2008). Origin and Physiological Roles of Inflammation.
Link: Cell
Neuroinflammation and Neurological Disorders
Heneka, M. T., et al. (2015). Neuroinflammation in Alzheimer’s Disease.
Link: The Lancet Neurology